Integrating COVID-19 Vaccination in Primary Care Service Delivery: Insights From Implementation Research in the Philippines
RTI International Philippines (Lava, de Claro, Lucero, Mendoza, Stan); Provincial Health Office, Province of Iloilo (Quiñon, Labis, Marcelo)
"The successful implementation of the integration process requires substantial government support at various levels, active community engagement, and a multisectoral approach to regulations and strategies."
Even before the COVID-19 outbreak, several studies had advocated for prioritising integrated health systems over fragmented ones that undermine the ability to withstand pandemics. A cohesive health system is resilient in that it facilitates the seamless integration of essential building blocks, including global health security (GHS), universal health care (UHC), and primary health care (PHC), within countries. In line with this approach, the Philippines enacted a UHC law in 2019 that aimed to establish an integrated health system. This article describe the design process, results, and lessons from implementing an integrated PHC model in the Philippines.
The Philippine Health Insurance Corporation's (PhilHealth) primary care benefit package, Konsulta, is an expanded set of preventive and promotive healthcare services that is made available to all Filipinos registered to accredited public and private primary care providers. Konsulta provided the avenue for designing an integrated service delivery model for service delivery and financing. The ReachHealth Project, funded by the United States Agency for International Development (USAID) and implemented by RTI International, provided technical support to the Provincial Government of Iloilo to develop and implement an integrated health service delivery model consisting of COVID-19 vaccination and family planning services alongside the primary care benefit package.
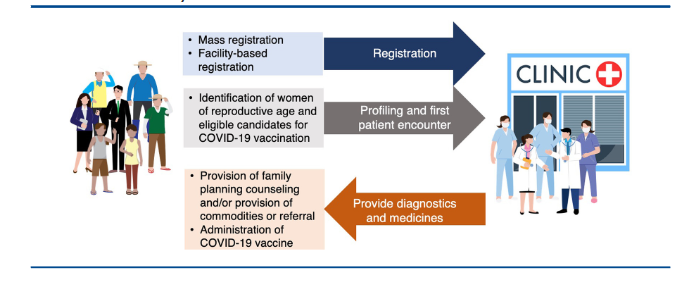
The ReachHealth Project was implemented in Iloilo by: (i) streamlining patient registration through mass registration or through facility-based registration; (ii) identifying women of reproductive age and eligible candidates for COVID-19 vaccination during the profiling and first patient encounter stage; and (iii) providing family planning counseling and services (onsite or through referral to a higher-level facility) and administering COVID-19 vaccines to those who want to receive these services. These interventions were implemented from October 2022 to April 2023.
This study uses a participatory implementation research approach. Quantitative data were collected from each primary care facility database, and 2 focus group discussions (FGDs) shed light on facilitators and barriers to implementation, adaptive measures taken, and alternative solutions to explore. A survey was also introduced in the last week of implementation to collect information on vaccine hesitancy. The researchers used the RE-AIM (reach, effectiveness, adoption, implementation, and maintenance) framework to organise the results and present the analysis.
The intervention showed substantial improvement across the 5 dimensions of the RE-AIM framework, including enhanced access to healthcare services, as indicated by improvements in primary care patient registration, family planning services, and COVID-19 vaccination processes, as well as an increase in registrations and first patient encounters. These improvements corresponded to sustained primary care facility participation throughout the study period: All 36 sites completed the implementation of the intervention during the entire study period.
In the 36 sites, the registration activities contributed to capturing 405,826 (19.8%) of the intended population, of which 100,795 (27.3%) underwent health profiling and received their initial patient consultation. Of these profiled individuals, 15,628 (14.1%) received COVID-19 vaccination; the integrated service delivery contributed to an additional 46.0% vaccinations of the set target. In addition, 10,369 (9.4%) of the profiled individuals received family planning counseling and services.
Findings from the vaccine hesitancy survey showed that of 2,427 respondents, 713 people (29.4%) expressed their primary concern as fear of experiencing side effects, and 548 people (22.6%) cited the nonavailability of their preferred vaccine as the reason for refusal. Challenges associated with expiration and maintaining cold chain storage during community-based activities further contributed to shaping this perception. In addition, 20.0% of respondents were undecided, indicating the potential role of family decision-makers in determining whether to proceed with vaccination..
The FGD participants identified several elements that were crucial for the successful integration of COVID-19 vaccination, including closely collaborating with community actors supporting community mobilisation activities, conducting information campaigns, allocating additional human resources for vaccination efforts, and ensuring the availability of sufficient vaccine supply and efficient logistics. They also reported barriers, such as insufficient backing from local leaders, resource constraints, negative community perception toward the programme, issues with the health information system, and inadequate national-level policy support and technical guidance.
In short, this study demonstrates "the promising potential for seamlessly integrating public health interventions within primary care settings, which serve as the first point of contact for individuals..." Specifically:
- The findings highlight the need for extensive governmental support at multiple levels (e.g., endorsement from local chief executives and local health authorities) to effectively implement integration. In addition, the national government should support enabling technologies to effectively capture and use data.
- COVID-19 has underscored the crucial role of community engagement and empowerment. Rather than imposing a predetermined implementation design from the outset, the ReachHealth team actively sought inputs from various stakeholders at different stages of the process. They found value in using a community-based approach to tackle vaccine hesitancy concerns and having local primary care practitioners play a pivotal role. A significant portion of the survey they conducted found common reasons that contribute to vaccine hesitancy that can be effectively addressed through persuasive communication by trusted primary care practitioners, community health workers, community centres, and local institutions that can foster vaccination equity.
- The team emphasises the importance of addressing the broader health determinants in establishing a comprehensive and integrated PHC system, which requires evidence-based policies and actions implemented in a multisectoral setting.
In conclusion: "This study adds to the existing global evidence on the value of integrated health care systems, specifically in low- and middle-income settings. It highlights the significance of a locally led, multisectoral, and contextually relevant approach to integration....Policymakers and implementers are encouraged to embed a learning system within intervention processes to foster continuous improvement, refine approaches, and explore strategies for integrated PHC."
Global Health: Science and Practice https://doi.org/10.9745/GHSP-D-23-00202.
- Log in to post comments
